Random mutations in genetic material may lead to bacteria resistant to a given antibiotic. When exposed to an antimicrobial, those individuals possessing resistant to the antimicrobial will have a selective advantage over other cells, and may reproduce at a faster rate. With rapid doubling times in bacteria, a resistant bacterium can proliferate into millions of cells in a short amount of time. In addition to proliferation of resistance by conventional binary fission, bacteria may also transfer resistance by means of genetic material. In bacteria, three methods of genetic transfer have been identified. These methods are conjugation, transduction, and transformation. The primary method of transfer of resistance is via conjugation, or plasmid transfer. Plasmids are short, circular pieces of DNA found within a bacterial cell. Plasmid types include R plasmids, which carry genes for resistance to specific antibiotics, and F plasmids, which confer the ability to transfer DNA to a cell lacking the F factor. A bacterium may carry resistance to several antibiotics on a given plasmid.
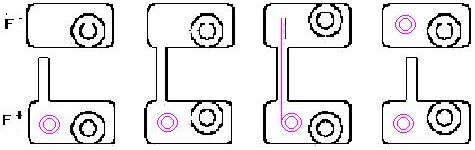
Basic mechanism of conjugation with F factor mediated transfer adapted from Prescott, Harley and Klein. First, the F+ bacterium forms a sex pilus, which joins with an F- cell. The plasmid is transferred through the sex pilus from the F+ cell to the F- cell. At the end of conjugation, both carry the fertility factor and are F+. If a gene conferring antibiotic resistance were present on the plasmid, both cells would now have resistance.

The figure(Right) illustrates possible mechanisms of transmission of resistant bacteria from live stock to human populations. First, the animal is fed subtherapeutic doses of antibiotics. Some of the animal's natural flora develop resistance to the antibiotic. In the presence of the antibiotic, those bacteria with resistance are favored over cells without the resistance. If a pathogen infects the animal.