Engineered cartilage
Grant to support tissue engineering for TMJ cartilage repair
10:27 a.m., Nov. 19, 2015--The temporomandibular joint, which joins the lower part of the jaw to the skull, is a source of pain and dysfunction for the 10 million Americans who suffer from TMJ disorders.
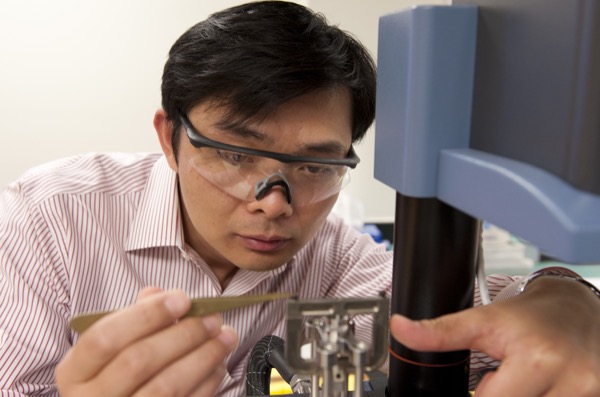
“TMJ problems are very painful, as we use this joint all the time for eating and talking,” says X. Lucas Lu, assistant professor of mechanical engineering at the University of Delaware. “It’s an important part of daily life, and it’s hard to ignore it when it doesn’t function correctly.”
Research Stories
Chronic wounds
Prof. Heck's legacy
Lu explains that TMJ disorders, which affect far more women than men, are often associated with cartilage degeneration. Because cartilage has a limited ability to regenerate itself, tissue engineering has become a promising therapeutic strategy for cartilage loss.
Lu and two UD colleagues, along with oral and maxillofacial surgeon John Vorrasi, recently received a grant from the Osteo Science Foundation to develop and test a new biomimetic material for TMJ cartilage repair.
Xinqiao Jia, associate professor of materials science and engineering, and Joe Fox, professor of chemistry and biochemistry, are designing and fabricating the novel material, Lu will test the material’s ability to generate new cartilage in the lab, and Vorrasi will help to evaluate the outcome of Lu’s experimental work.
Lu explains that one of the challenges in treating TMJ disorders is that the condylar cartilage in this joint has a drastically different structure from the hyaline cartilage found in other joints like the knee.
“TMJ condylar cartilage is made up of a unique fibrous superficial layer, composed of mainly collagen fibers, covering the hyaline cartilage,” he says. “Our recent research revealed that this fibrous layer is essential for the mechanical function and lubrication of TMJ condyle in daily functions. To be effective, engineered condylar cartilage will have to incorporate the structural heterogeneity displayed by this native tissue.”
The Fox-Jia team is developing a tissue-mimicking synthetic matrix employing their recently established interfacial bioorthogonal polymerization techniques. Bioorthogonal chemistry enables biomolecules to be tracked in their native environment, laying the foundation for breakthroughs in tissue engineering.
“The biomimetic matrix will provide the resident stem cells with spatially controlled cues to guide the establishment of appropriate tissue structures for TMJ repair,” Jia says. “We expect that the regenerated tissue will function similarly to native condylar cartilage and meet the mechanical requirement of daily TMJ activities.”
Vorrasi, who is the residency program director for oral and maxillofacial surgery at Christiana Care, is optimistic about the potential for the research to move from benchtop and fundamentals to clinical application.
“My dilemma as a clinician is to find less invasive techniques and to optimize good outcomes for TMJ surgery,” he says. “This project represents the first effort to fabricate a biomimetic matrix for TMJ condylar cartilage repair by replicating the unique anatomy of the native tissue.”
Article by Diane Kukich
Photo by Kathy F. Atkinson