Combating cancer
Biomedical engineering faculty receive funding for research on metastatic breast cancer
9:16 a.m., April 21, 2016--Tremendous advances in the detection and treatment of cancer over the past four decades have led to a significant increase in the five-year survival rate, yet the ability to prevent, diagnose and treat metastatic cancer remains a significant hurdle in reducing cancer-associated mortality.
“Metastasis, or the spread of cancer from one organ or part of the body to another, is responsible for 90 percent of cancer mortality,” says John Slater, assistant professor in the Department of Biomedical Engineering at the University of Delaware. “This statistic points to a critical need for better metastasis models, diagnostic tools and treatment strategies.”
Research Stories
Chronic wounds
Prof. Heck's legacy
Slater and Emily Day, also an assistant professor of biomedical engineering, recently received funding from the American Cancer Society to explore this issue.
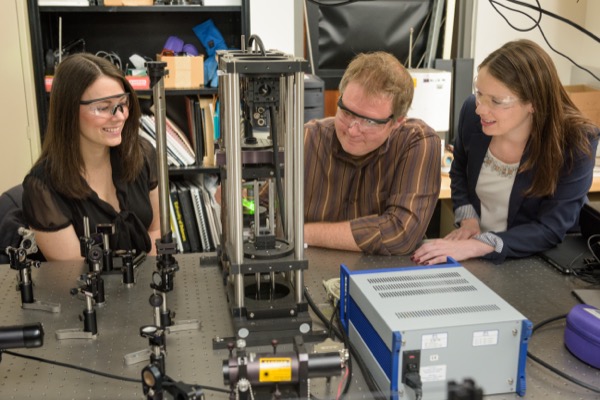
Slater’s project, “A Three-Dimensional, Cardio and Lymphatic Vascularized in Vitro Metastasis Model,” focuses on developing a hydrogel-based model that mimics the metastatic environment. The device will allow for direct visualization and quantification of the multistep processes that occur during metastasis.
Successful completion of the model will allow for future studies to gain insight into the molecular mechanisms and environmental factors that drive metastasis. The model will also provide a foundation for the development of a diagnostic tool to quantify the potential for a patient’s cancer to metastasize and the creation of personalized treatment strategies.
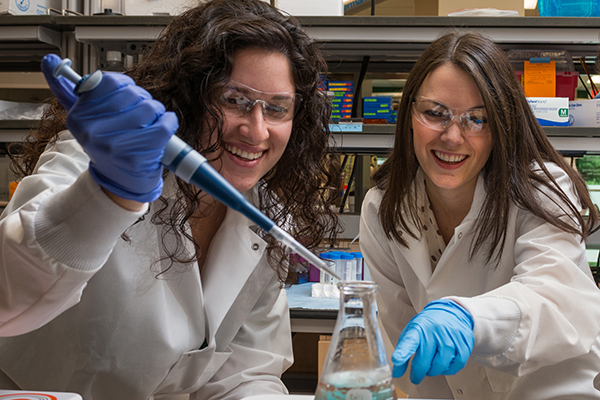
Day’s project, “Elucidating the Impact of Wnt Inhibitory Nanoparticles on Metastatic Potential of Breast Cancer Cells,” is aimed at developing a treatment for metastatic breast cancer. She explains that signaling initiated by a family of molecules called Wnt proteins is a key driving force behind breast cancer metastasis. Her plan is to halt this signaling pathway with nanoparticles coated with antibodies and small interfering RNA (siRNA) molecules.
“Our hope is that the antibodies will enable the nanoparticles to selectively bind breast cancer cells rather than normal cells and the siRNA molecules will suppress Wnt signaling in the cancer cells, thereby reducing their metastatic potential,” she says.
She and her team will evaluate these nanoparticles as a treatment for metastatic breast cancer by assessing their impact on cellular gene expression and determining their impact on breast cancer cell viability and migration.
About the grants
Slater and Day each received $30,000 from the American Cancer Society via the Institutional Research Grant program. This support, which is granted to researchers within six years of their first academic appointment, is aimed at allowing awardees to obtain preliminary results that will enable them to compete successfully for peer-reviewed national grants in cancer research.
Article by Diane Kukich